Frequently Asked Questions
It has been scientifically determined that chronic pain is a belief/brain function and not necessarily a sign of tissue damage. This means that altering your thoughts, beliefs, practices can reduce or even eliminate your pain.
Target each of these specific components of pain to get relief: (see ‘How do some experts explain the understanding of pain? FAQ, for more on the these components.)
EMOTION/ AFFECTIVE-MOTIVATIONAL
- Hopefulness–Look for the positive side of situations
- Deal with past trauma and fears
- Engage in fun, enjoyable activities
- Consider treatment for depression and/or anxiety
- Stay or get connected with a community
COGNITION/ EVALUATIVE-COGNITIVE
- Study and learn how pain is constructed in our brains and how pain is meant to be our protector (Try this 1.5 hour course: “Why We Hurt and What to do About It“)
- Mindfulness Techniques, Relaxation training, Meditation
- Cognitive Behavior Therapy
SENSATION/ SENSORY-DISCRIMINATIVE
- Breathing Techniques like diaphragmatic, deep breathing and/or Square Breathing.
- Walking and other exercise for strength, endurance, and flexibility
- Adequate sleep and a balanced diet
- A personal story of sensory-discrimination can be found here.
You can see additional examples of helpful practices by exploring the Life Stories in the Resources Search tab and from the Valued References tab.
The RESOURCE SEARCH TABLE is a curated archive of videos, books, articles, and presentations featuring member’s and clinician’s stories describing their journey with and insights of pain science research, and how their views and practices changed. These resources go though multiple steps by a number of individuals for vetting purposes before making their way on this website.
Each resource presented on the Resource Table is accompanied by the following:
- Resource Identification Number
- Title linking to the resource page
- Author information including designation and general background
- Synopsis = 1-2 written paragraphs covering the presentation’s content
- Summary = two page written summary of the presentation
- Evaluation = Staff description of the presentation from their personal standpoint of its inherent value
- Complete Transcript (for visual and audio presentation)
- Type and Length of the resource
- And a link for an outside resource, or a single-click access to an instance of the resource.
As the resources increase in number, this resource table has the state-of-the-art search capacity to help you quickly find the research subjects you are looking for. All element within the resource table is included in the search criterial.

- Ask your clinician their knowledge of recent Pain Science insights. (This could be a shared learning experience with your clinician.)
- Be honest about the pain you are experiencing and the information you are learning about pain science.
- Ask if there are any other conditions to be ruled out as causes of your pain.
- Ask how long it usually takes for a person to recover from your surgery and/or injuries so you can be confident it’s safe to increase your activity level.
- Ask for guidance with increasing your daily activity level.
- Be honest about the pain medications you are taking and ask about side-effects with prolonged use.
After multiple surgeries during a lifetime of dealing with pain, our story teller, Mo, knows what gives her relief.
What Mo has learned to do:
- Keep in mind that it takes time to change the brain so it does not perceive that you are in danger and knows that you don’t need your brain to send out pain to protect you. This takes work and practice.
- Deep breathing (Diaphragmatic Breathing) and its many benefits.
- Movement & Pacing: If you can only move a few feet, do that and then move little farther each time
- Mindfulness: Keep your mind on your surroundings, not your pain
- Perception: If you perceive it will hurt, it will hurt.
- Visualization: Set goals and see yourself accomplishing a task
- Gratitude and forgiveness
Books that helped her along her journey:
- How Emotions are Made: The Secret Life of the Brain by Lisa Feldman Barrett
- The Confidence Gap by Russ Harris
- The Happiness Trap by Russ Harris
- MBSR |Mindfulness-Based Stress Reduction Daily Practices From the Heart of Mindfulness-Based Stress Reduction by ElishaGoldstein,PHD & Bob Stahl, PHD (This book shows is the heart of mindfulness. It reveals how the power of being present the deepening of our own awareness and the building of our own reliance will help us ride the ever changing and growing complicated world. This book will help you settle down and settle into the deeper and more tenacious part of who you are the part you have probably been looking for all along, by Tim Ryan)
Formed in 2018, the Oregon Pain Science Alliance (the Alliance) is an all-volunteer nonprofit 501(c)3 corporation. Our members come from the health care community, their patients, and others who follow pain science research. We seek to share current information on how pain experiences are formed in the brain and influenced by biological, psychological, and/or social factors, along with practices we have found helpful and consistent with pain science concepts.
The PainScienceLifeStories.com website provides access to our video archive featuring community member’s and clinician’s stories describing their journey to embrace the insights of pain science research, and how their practices changed. Also included are links to other pain science explanations and practices we have found useful. We curate all archive resources with features to aid the user in finding answers to their questions.
The archive is not exclusive to stories we produce, so if you know of, or have a pain science life story, please use the contacts below to collaborate with us.
Phone: 541-224.8378
Email: opsa@painsciencelifestories.org
- International Association for the Study of Pain (IASP):
Pain is “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
- Dr. Kevin Cuccaro, D.O.:
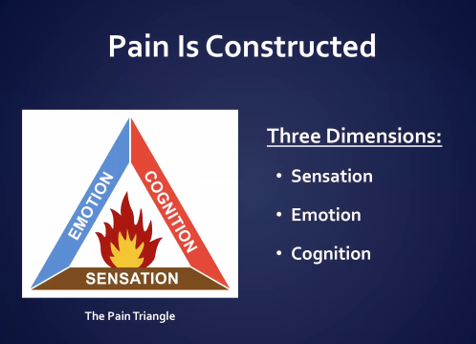
THE PAIN TRIANGLE
MASTERY CONCEPT #1: PAIN = PROTECTION
Pain cannot be explained by bodily damage. The person’s perceived danger is the key to their pain.
MASTERY CONCEPT #2: All Pain comes from the Brain (not from the Body).
Pain is a dynamic process constructed in the brain from three elements imagined as a triangle: (1) cognitive/evaluative (HEAT), (2) affective/ motivational (OXYGEN), and (3) sensory/discriminative (FUEL). Just as fire fighters understand that a fire burns only in the presence of heat, oxygen, and fuel, the Pain Triangle’s three elements are the combined source of pain. Firefighters put out fires by eliminating oxygen, heat, or fuel. Likewise, people experiencing pain can use their understanding of the Pain Triangle to “deconstruct” their pain fire. They master their pain by dealing with its cognitive, sensory, and/or emotional aspects.
MASTERY CONCEPT #3: If you understand what you are treating, you can treat it.
Risk factors for pain, anxiety, depression, substance abuse are all the same.
Strong belief that pain = damage creates increased pain.
Endorphins are our body’s natural opioid system, so if a person takes opioids their reactivity to threat (i.e. their pain) increases.
- Lorimer Moseley, DSc, PhD, FACP and David S. Butler BPhty MAppSc EdD
THE GRAND POOBAH PAIN THEORY (GPPT)
- Pain is an unpleasant feeling that is felt somewhere in the body and urges us to protect that bodily location.
- Pain is one of many protective mechanisms. Others include movement, immune, cognitive, endocrine and autonomic.
- Pain is the only protective mechanism we are necessarily aware of and compels us to do something to protect the painful bit.
- Pain is modulated by any credible evidence that protection is warranted.
The exact level of an individual’s pain cannot be directly measured or known by their care provider. Pain has to be gauged by the individual themselves. A variety of questionnaires and rating scales may be used to identify a person’s pain level and when it changes. None of these methods can be used to compare the pain of one individual to another. Commonly used subjective ways to measure pain and its effects include: 0-10 Pain Scale, Brief Pain Inventory Diagram, PEG-3 Pain Screening Tool, Keele STarT Back Tool, Oswestry Low Back Pain Disability Questionnaire, and Pain Catastrophizing Scale.
Pain science is the study of the nature of pain, its treatment, and related pain-management practices. In recent years, our understanding of how pain works has grown and changed due to ongoing research, revealing a better understanding of the pain experience and its management. Now the understanding is that pain is not simply the consequence of biomechanical tissue damage. As revealed by neuroscience research in recent decades, pain is a protective response our brains produce, which is influenced by many BioPsychoSocial factors, particularly the individual’s pain beliefs. Therefore tissue damage may be a factor, but is not always present when pain is experienced.
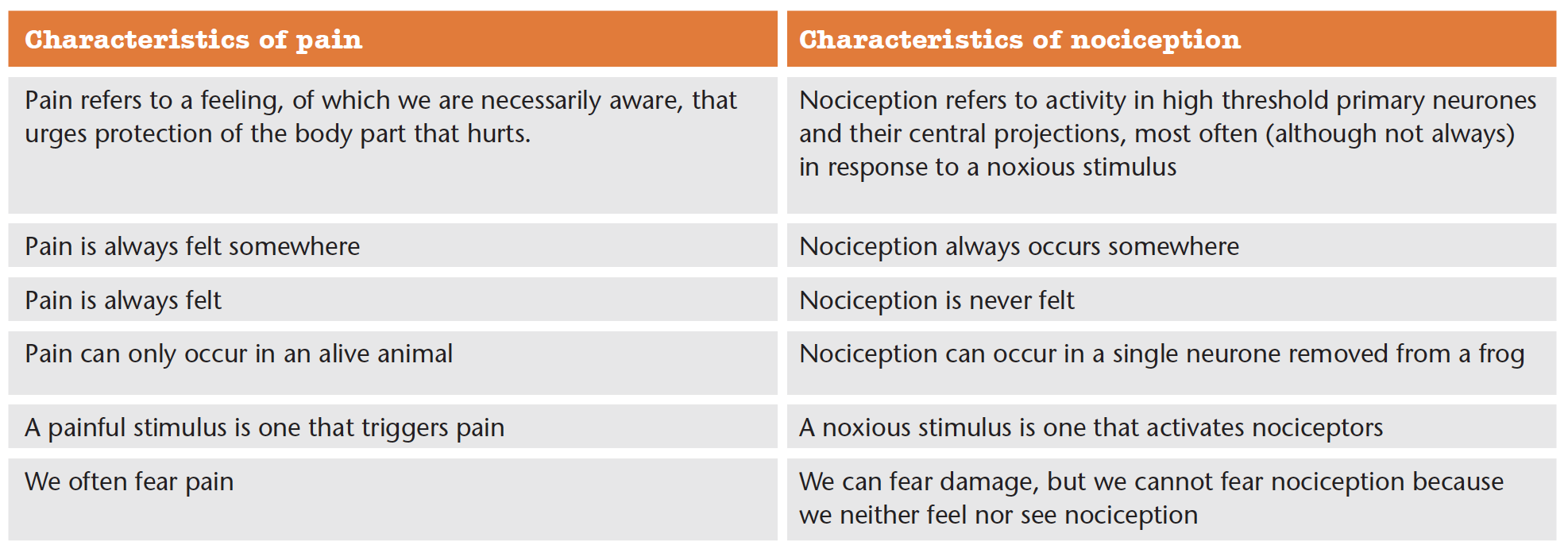
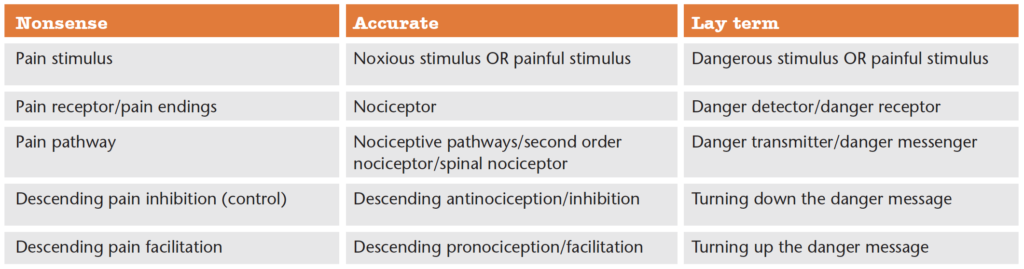
Image credit: https://www.noigroup.com/noijam/two-tables/
Phantom limbs are a common experience for those who have lost a limb, wherein they feel the limb as though it is still attached to them. In some of these cases, the individual will feel pain in their phantom limb. Phantom pain is a form of neuropathic pain.
Basbaum, Allan I., 2012. The Science of Pain, University of California Television (UCTV)